%20IF%20Banner%202025.svg)
(Toronto, ON, June 19, 2025) JMIR Publications is pleased to announce that JMIR Rehabilitation and Assistive Technologies has achieved its inaugural Journal Impact Factor of 3.0, as published in the Journal Citation Reports (JCR) 2025 from Clarivate.
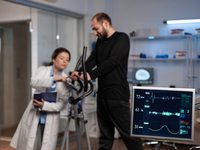
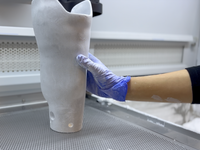
This significant achievement highlights the growing influence and importance of research in rehabilitation, physiotherapy and assistive technologies, robotics, prosthetics and implants, mobility and communication tools, home automation, and telerehabilitation. The inaugural Journal Impact Factor for JMIR Rehabilitation and Assistive Technologies reflects the high-quality and impactful research in this unique field. This achievement also underscores the collective commitments and contributions of authors, peer reviewers, editors, and journal staff, along with the dedicated leadership of the journal’s editor in chief, Sarah Munce, MSc, PhD, implementation scientist at Holland Bloorview Kids Rehabilitation Hospital, Bloorview Research Institute and assistant professor at Institute of Health Policy, Management and Evaluation (IHPME), Rehabilitation Sciences Institute (RSI), University of Toronto.
Here is a selection of the top-cited articles in JMIR Rehabilitation and Assistive Technologies as recognized in the Journal Citation Reports 2025 from Clarivate:
- Shah N, Costello K, Mehta A, Kumar D. Applications of Digital Health Technologies in Knee Osteoarthritis: Narrative Review. JMIR Rehabil Assist Technol 2022;9(2):e33489 (doi: 10.2196/33489)
- Arntz A, Weber F, Handgraaf M, Lällä K, Korniloff K, Murtonen KP, Chichaeva J, Kidritsch A, Heller M, Sakellari E, Athanasopoulou C, Lagiou A, Tzonichaki I, Salinas-Bueno I, Martínez-Bueso P, Velasco-Roldán O, Schulz RJ, Grüneberg C. Technologies in Home-Based Digital Rehabilitation: Scoping Review. JMIR Rehabil Assist Technol 2023;10:e43615 (doi: 10.2196/43615)
- Dinesen B, Hansen HK, Grønborg GB, Dyrvig AK, Leisted SD, Stenstrup H, Skov Schacksen C, Oestergaard C. Use of a Social Robot (LOVOT) for Persons With Dementia: Exploratory Study. JMIR Rehabil Assist Technol 2022;9(3):e36505 (doi: 10.2196/36505)
JMIR Rehabilitation and Assistive Technologies also recently received a 2024 CiteScore of 5.7, ranking Q1 (#11 of 165, 93rd percentile) in the “Medicine: Rehabilitation” category, and Q1 in the “Health Professions: Physical Therapy, Sports Therapy and Rehabilitation” category. CiteScore is a 4-year average of citations, based on Elsevier Scopus data.
JMIR Rehabilitation and Assistive Technologies’ ranking will appear in the October 2025 update Journal Citation Reports (JCR) from Clarivate. Due to technical delays in indexing on Clarivate’s side, some content was missing from the Web of Science at the time of JCR data extraction.
Clarivate has since received all the missing articles that were required to calculate the Journal Impact Factor. Projected metrics for the journal are posted on the Help page and can be considered official.
JMIR Rehabilitation and Assistive Technologies will be listed in the category page with its new ranking in JCR’s October reload, and the journal’s profile page will then include the full 2024 profile data.
To view a full list of JMIR Publications journals with a Journal Impact Factor, please visit the website.
JMIR Publications recommends that authors and other parties consider alternative metrics, in combination with Journal Impact Factor, when assessing a journal’s standing and impact. While proud of its Journal Impact Factor rankings, JMIR Publications discourages misuse of citation-based impact scores.
Source: Journal Citation Reports 2025 from Clarivate